Ever wonder why some days you feel energized and focused, while others leave you dragging? The answer might be flowing through your veins right now: blood sugar.
Blood sugar, or blood glucose, is more than just a number on a medical chart. It’s the fuel that powers our cells, influences our mood, and impacts our overall health.
Whether you’re dealing with diabetes or simply aiming for optimal wellness, understanding blood sugar is crucial. Let’s dive into the sweet (and sometimes not-so-sweet) world of glucose and discover how it affects your daily life.
This article is brought to you by Health Nutrition – your complete health and wellness community. Health Nutrition offers everything you need to achieve your goals and live a fitter, healthier, happier life, all in one place. From personalized diet and exercise plans to one-on-one guidance from health coaches, Health Nutrition supports you every step of the way.
What is Blood Sugar and Why Does it Matter?
Blood sugar is exactly what it sounds like: sugar in your blood. But it’s not the table sugar you stir into your coffee. We’re talking about glucose, the primary source of energy for your body’s cells.
When you eat, your digestive system breaks down carbohydrates into glucose. This glucose enters your bloodstream, causing your blood sugar levels to rise.
Why does this matter? Well, imagine glucose as the gasoline for your body’s engine. Too little, and you might stall out. Too much, and you could damage the engine.
Maintaining the right balance of blood glucose levels is crucial for your body to function optimally. It affects everything from your energy and mood to your long-term health prospects.
The Basics of Blood Sugar Regulation
Your body has a sophisticated system for regulating blood sugar. At the heart of this system is a hormone called insulin.
Think of insulin as a tiny key that unlocks your cells, allowing glucose to enter and be used for energy. When your blood sugar rises, your pancreas releases insulin to help move that glucose into your cells.
Another hormone, glucagon, works in the opposite direction. When your blood sugar dips too low, glucagon signals your liver to release stored glucose, bringing your levels back up.
This delicate dance of hormones and glucose is happening in your body 24/7, keeping your blood sugar levels within a healthy range. Pretty amazing, right?
Understanding Blood Sugar Levels

So, what exactly constitutes “normal” blood sugar levels? It’s not a one-size-fits-all answer, but there are general guidelines.
For most people without diabetes, a fasting blood sugar (measured first thing in the morning before eating) should be below 100 mg/dL. Two hours after eating, it should be below 140 mg/dL.
These numbers can vary slightly based on factors like age, overall health, and specific medical conditions. That’s why it’s essential to work with your healthcare provider to understand what’s normal for you.
Remember, blood sugar isn’t static. It naturally fluctuates throughout the day in response to meals, exercise, stress, and other factors.
The goal isn’t to maintain a perfectly flat line, but rather to avoid extreme highs and lows. Think of it like keeping a boat steady in gently rolling waves, rather than in a storm-tossed sea.
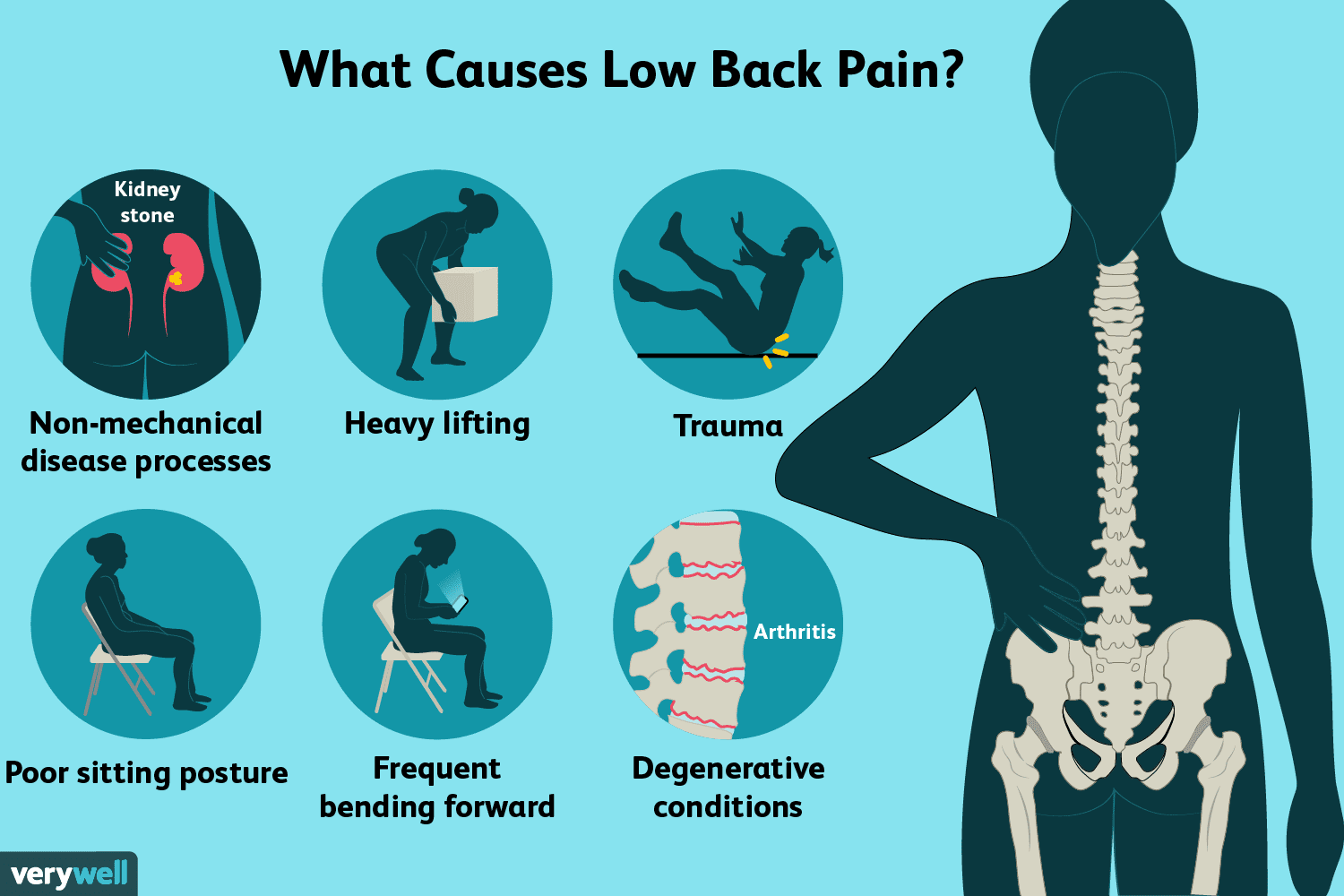
High Blood Sugar: Causes and Risks
High blood sugar, or hyperglycemia, occurs when there’s too much glucose circulating in your bloodstream. It’s like having too much fuel in your car’s engine – it can cause problems if left unchecked.
Common causes of high blood sugar include eating more carbohydrates than usual, not taking enough insulin (for those with diabetes), illness, stress, or certain medications.
In the short term, high blood glucose can cause symptoms like increased thirst, frequent urination, blurred vision, and fatigue. It’s your body’s way of trying to flush out the excess sugar.
Long-term, chronic high blood sugar can lead to serious health complications. These include heart disease, kidney damage, nerve problems, and vision issues.
That’s why it’s crucial to catch and address high blood sugar early. Regular monitoring and lifestyle adjustments can go a long way in preventing these potential complications.
Low Blood Sugar: Symptoms and Management
On the flip side, low blood sugar, or hypoglycemia, occurs when your blood glucose drops below normal levels. It’s like running your car on fumes – you might sputter and stall.
Common symptoms of low blood sugar include shakiness, sweating, confusion, irritability, and in severe cases, loss of consciousness. It’s often described as feeling “hangry” (hungry + angry) on steroids.
Low blood sugar can be caused by skipping meals, excessive exercise, or taking too much diabetes medication. For people without diabetes, it’s less common but can occur after prolonged fasting or intense physical activity.
If you experience symptoms of low blood sugar, the quickest fix is to consume something with fast-acting carbohydrates. A small glass of fruit juice or a few glucose tablets can help raise your blood sugar quickly.
The Role of the American Diabetes Association
When it comes to blood sugar management, the American Diabetes Association (ADA) is a powerhouse of information and support. They’re like the wise grandparent of the diabetes world, offering guidance based on years of research and experience.
The ADA sets standards for diabetes care that healthcare providers across the country follow. They fund critical research, advocate for patients’ rights, and provide educational resources for people living with diabetes.
But you don’t have to have diabetes to benefit from the ADA’s wisdom. Their guidelines on nutrition, exercise, and overall health can be valuable for anyone looking to maintain healthy blood sugar levels.
The ADA’s website is a treasure trove of information, from recipes to risk assessment tools. It’s worth bookmarking for future reference as you continue your blood sugar journey.
Effective Blood Sugar Control Strategies

Controlling your blood sugar isn’t about perfection – it’s about progress. Small, consistent steps can lead to big improvements in your overall health.
The key is to find a balance that works for you. This might involve a combination of diet changes, exercise, medication (if prescribed by your doctor), and stress management techniques.
Remember, what works for one person might not work for another. It’s all about finding your personal sweet spot (pun intended) when it comes to blood sugar management.
Let’s explore some strategies that can help you keep your blood sugar levels in check. With a little knowledge and effort, you’ll be well on your way to better blood sugar control.
And don’t forget – it’s okay to have occasional treats or days when things don’t go as planned. The goal is overall consistency, not perfection.
Dietary Approaches for Blood Sugar Management
When it comes to managing blood sugar through diet, it’s not just about cutting out sugar. It’s about making smart choices that help keep your glucose levels stable.
One effective approach is to focus on low glycemic index (GI) foods. These are foods that cause a slower, more gradual rise in blood sugar. Think whole grains, legumes, and most fruits and vegetables.
Balancing your plate is another key strategy. Aim for a mix of lean protein, healthy fats, and complex carbohydrates at each meal. This combination helps slow down digestion and prevent rapid spikes in blood sugar.
Portion control is also crucial. Even healthy foods can raise blood sugar if eaten in large quantities. Using smaller plates or measuring portions can be helpful tricks.
Don’t forget about the power of fiber. It not only aids digestion but also helps regulate blood sugar absorption. Aim to include plenty of high-fiber foods in your diet.
Exercise and Physical Activity for Blood Sugar Control
Exercise is like a secret weapon for blood sugar control. It helps your body use insulin more effectively, lowering your blood glucose levels both during and after your workout.
You don’t need to run marathons to see benefits. Even a brisk 30-minute walk can make a difference. The key is consistency – aim for at least 150 minutes of moderate-intensity exercise per week.
Resistance training, like weightlifting or bodyweight exercises, can be particularly effective. It helps build muscle, which in turn helps your body process glucose more efficiently.
Remember to stay hydrated during exercise, and if you have diabetes, check your blood sugar before, during, and after intense workouts. Always consult with your healthcare provider before starting a new exercise regimen.
Monitoring Blood Sugar: Tools and Techniques
Keeping tabs on your blood sugar doesn’t have to feel like a full-time job. Thanks to modern technology, there are more options than ever for convenient and accurate monitoring.
The most common method is using a glucose meter, which requires a small blood sample from a fingertip. It’s quick, relatively painless, and provides immediate results.
For those who need more frequent monitoring, continuous glucose monitors (CGMs) are game-changers. These small devices, worn on the body, provide real-time glucose readings throughout the day and night.
Some CGMs can even send alerts to your smartphone if your blood sugar goes too high or low. It’s like having a personal blood sugar bodyguard!
Regardless of the method you choose, the key is consistency. Regular monitoring helps you understand your body’s patterns and make informed decisions about diet, exercise, and medication.
The Importance of Regular Blood Sugar Checks
Checking your blood sugar regularly is like taking the pulse of your overall health. It provides valuable insights into how your body responds to different foods, activities, and stressors.
For people with diabetes, regular checks are crucial for managing their condition and preventing complications. But even if you don’t have diabetes, occasional checks can be beneficial.
Regular monitoring can help you spot patterns. Maybe you notice your blood sugar spikes after certain meals, or dips when you’re stressed. This information empowers you to make adjustments.
Remember, knowledge is power. The more you know about your blood sugar patterns, the better equipped you are to make informed decisions about your health.
Understanding Diabetes and Its Connection to Blood Sugar
Diabetes and blood sugar are like two sides of the same coin. At its core, diabetes is a condition where the body struggles to regulate blood sugar effectively.
In type 1 diabetes, the body doesn’t produce insulin, the key hormone for blood sugar regulation. It’s like having a car without a gas pedal – you can’t control the flow of fuel (glucose) into your cells.
Type 2 diabetes, the most common form, is different. Here, the body becomes resistant to insulin or doesn’t produce enough. It’s like having a faulty gas pedal that doesn’t respond properly.
Managing diabetes is all about keeping blood sugar levels as close to normal as possible. This often involves a combination of medication, diet changes, exercise, and regular monitoring.
But here’s the good news: with proper management, people with diabetes can lead full, healthy lives. It’s all about understanding your body and giving it the care it needs.
Types of Diabetes: Type 1, Type 2, and Gestational
Diabetes isn’t a one-size-fits-all condition. There are several types, each with its own characteristics and challenges.
Type 1 diabetes is an autoimmune condition where the body attacks its own insulin-producing cells. It usually develops in childhood or early adulthood and requires lifelong insulin therapy.
Type 2 diabetes, the most common form, typically develops later in life. It’s often linked to lifestyle factors like diet and physical activity, though genetics play a role too.
Gestational diabetes occurs during pregnancy and usually resolves after childbirth. However, it increases the risk of developing type 2 diabetes later in life.
Understanding which type of diabetes you have is crucial for proper management. Each type requires a tailored approach to treatment and lifestyle modifications.
Medications and Treatments for Blood Sugar Control
When it comes to managing blood sugar, sometimes lifestyle changes aren’t enough. That’s where medications come in, offering a helping hand in the battle for glucose control.
For type 1 diabetes, insulin is the cornerstone of treatment. It’s like providing the body with the key it needs to unlock cells and let glucose in.
Type 2 diabetes has a wider range of medication options. Some help the body use insulin more effectively, while others reduce glucose production or slow its absorption.
Newer medications, like GLP-1 receptor agonists, work by mimicking natural hormones that regulate blood sugar. They’re like traffic cops, helping to direct glucose where it needs to go.
Remember, medication is just one piece of the puzzle. It works best when combined with healthy eating, regular exercise, and consistent monitoring.
Insulin Therapy: When and How It’s Used
Insulin therapy is a lifeline for people with type 1 diabetes and many with advanced type 2 diabetes. It’s like giving your body back the key it needs to unlock energy from glucose.
There are several types of insulin, from rapid-acting to long-acting. Each type has its own onset, peak, and duration, allowing for customized treatment plans.
Insulin can be delivered via injections or an insulin pump. Pumps offer more flexibility, delivering small amounts of insulin throughout the day to mimic the body’s natural processes.
While insulin therapy requires careful management to avoid low blood sugar, it’s a powerful tool for maintaining glucose control. With proper education and support, many people find it becomes a manageable part of their daily routine.
Lifestyle Factors Affecting Blood Sugar
Your blood sugar isn’t just affected by what you eat. A whole host of lifestyle factors can influence those glucose levels.
Stress, for instance, can cause your blood sugar to rise. It’s like your body preparing for a “fight or flight” situation, releasing extra glucose for energy.
Sleep plays a crucial role too. Poor sleep can lead to insulin resistance, making it harder for your body to regulate blood sugar effectively.
Even the time of day can impact your blood sugar. Many people experience higher morning blood sugar due to hormonal changes overnight – a phenomenon known as the “dawn effect.”
Understanding these factors can help you make informed decisions about your daily habits. Small changes, like prioritizing sleep or finding stress-relief techniques, can have a big impact on your blood sugar control.
Stress Management and Blood Sugar Control
Stress and blood sugar are more closely linked than you might think. When you’re stressed, your body releases hormones that can cause your blood sugar to rise.
Finding effective stress management techniques isn’t just good for your mental health – it’s crucial for your blood sugar control too. This could include meditation, deep breathing exercises, or regular physical activity.
Some people find that creative activities, like art or music, help them unwind. Others might prefer spending time in nature or practicing yoga.
Remember, what works for one person might not work for another. The key is to find stress-relief methods that resonate with you and make them a regular part of your routine.
Potential Complications of Uncontrolled Blood Sugar
While it’s not pleasant to think about, understanding the potential complications of uncontrolled blood sugar can be a powerful motivator for taking care of your health.
Over time, high blood sugar can damage blood vessels and nerves throughout your body. This can lead to a range of issues, from heart disease and stroke to kidney problems and vision loss.
Diabetes, if not well-managed, can increase the risk of foot problems. Poor circulation and nerve damage can make it harder to notice and heal from injuries.
The good news? Many of these complications are preventable with good blood sugar control. It’s never too late to start taking steps towards better health.
Remember, knowledge is power. By understanding these risks, you’re better equipped to take proactive steps to protect your health.
Prevention and Early Detection of Blood Sugar Issues
When it comes to blood sugar issues, prevention is truly the best medicine. Regular check-ups with your healthcare provider can catch potential problems early, before they become serious.
Know your risk factors. Family history, age, and certain ethnic backgrounds can increase your likelihood of developing diabetes. If you’re at higher risk, more frequent screenings may be recommended.
Pay attention to warning signs. Increased thirst, frequent urination, unexplained weight loss, or blurred vision could be red flags for blood sugar issues. Don’t ignore these symptoms – talk to your doctor.
Lifestyle choices play a huge role in prevention. Maintaining a healthy weight, staying active, and eating a balanced diet can significantly reduce your risk of developing type 2 diabetes.
Remember, small changes can make a big difference. Even modest weight loss and increased physical activity can help prevent or delay the onset of type 2 diabetes in high-risk individuals.
The Power of Knowledge: Educating Yourself About Blood Sugar
Understanding your blood sugar is like learning a new language – it opens up a whole new world of health insights. The more you know, the better equipped you are to make informed decisions.
Don’t be afraid to ask questions. Your healthcare team is there to help you understand your body and your health. No question is too small or too silly when it comes to your well-being.
Consider joining a support group or online community. Sharing experiences with others who are on similar journeys can be incredibly valuable and encouraging.
Stay up-to-date with the latest research and recommendations. The field of diabetes and blood sugar management is constantly evolving, with new insights and treatment options emerging regularly.
Remember, knowledge is empowering. The more you understand about blood sugar, the more control you have over your health and your life.
Tools and Resources for Blood Sugar Management
In today’s digital age, there’s a wealth of tools and resources available to help you manage your blood sugar effectively. From smartphone apps to online calculators, technology can be a powerful ally in your health journey.
Many glucose meters now sync with smartphone apps, allowing you to track your readings over time and spot patterns easily. Some apps even provide personalized insights based on your data.
Meal planning tools can help you make smart food choices. Look for apps or websites that provide nutritional information and help you balance your carb intake throughout the day.
Don’t underestimate the power of a good old-fashioned journal. Keeping track of your meals, exercise, and blood sugar readings can help you and your healthcare team make informed decisions about your care.
Living Well with Healthy Blood Sugar Levels
Maintaining healthy blood sugar levels isn’t just about avoiding complications – it’s about living your best life. When your blood sugar is well-controlled, you’re likely to feel more energetic, focused, and emotionally balanced.
Remember, perfection isn’t the goal. There will be ups and downs, and that’s okay. What matters is your overall trend and how you feel day to day.
Celebrate your successes, no matter how small. Did you resist a tempting dessert? Go for a walk instead of watching TV? These small victories add up over time.
Don’t let blood sugar management define you. It’s an important part of your health, but it doesn’t have to be the center of your life. Find a balance that works for you and allows you to enjoy life to the fullest.
With the right knowledge, tools, and support, you can take control of your blood sugar and pave the way for a healthier, happier future.
The Role of Support Systems in Blood Sugar Management
Managing your blood sugar doesn’t have to be a solo journey. In fact, having a strong support system can make a world of difference in your health outcomes.
Family and friends can be powerful allies. Educate them about your health needs and how they can support you. Sometimes, just having someone to talk to can make a big difference.
Consider joining a support group, either in-person or online. Sharing experiences with others who understand your challenges can be incredibly validating and motivating.
Your healthcare team is a crucial part of your support system. Build a good relationship with them, and don’t hesitate to reach out when you have questions or concerns.
Looking to the Future: Innovations in Blood Sugar Management
The field of blood sugar management is constantly evolving, with exciting innovations on the horizon. From smarter continuous glucose monitors to artificial pancreas systems, technology is changing the game.
Researchers are exploring new medications that could make blood sugar management easier and more effective. Some are even investigating potential cures for type 1 diabetes.
Personalized medicine is becoming increasingly important. In the future, treatments might be tailored even more precisely to your individual needs and genetic profile.
While these advancements are exciting, remember that the basics of good health – a balanced diet, regular exercise, and consistent monitoring – will always be important.
Stay curious and open to new developments. The future of blood sugar management looks brighter than ever!
Embracing a Holistic Approach to Blood Sugar Health
Managing your blood sugar isn’t just about numbers on a meter. It’s about embracing a holistic approach to your overall health and well-being.
Consider how factors like stress, sleep, and emotional health impact your blood sugar. Addressing these areas can lead to better glucose control and improved quality of life.
Don’t neglect other aspects of your health. Regular check-ups, dental care, and eye exams are all important parts of maintaining your overall well-being.
Remember, you’re more than your blood sugar levels. Focus on nourishing your body, moving in ways you enjoy, and finding balance in all areas of your life.
By taking a comprehensive approach to your health, you’re setting yourself up for success in managing your blood sugar and living your best life.
A Final Word on Blood Sugar Supplements
Before we part ways, it’s worth mentioning that there are supplements available that may support healthy blood sugar levels. One such product is Blood Sugar Plus, offered by Health Nutrition.
Blood Sugar Plus is designed to support healthy blood sugar levels naturally. It also aims to aid the body’s natural immune function, which is an important aspect of overall health.
What sets Blood Sugar Plus apart is its commitment to being 100% natural and vegan friendly. This makes it a potential option for those looking for a plant-based approach to blood sugar support.
As with any supplement, it’s crucial to consult with your healthcare provider before adding Blood Sugar Plus or any new product to your regimen. They can help you determine if it’s appropriate for your individual health needs.
Remember, supplements should complement, not replace, a healthy diet and lifestyle. They’re just one tool in your blood sugar management toolkit!
Source link